
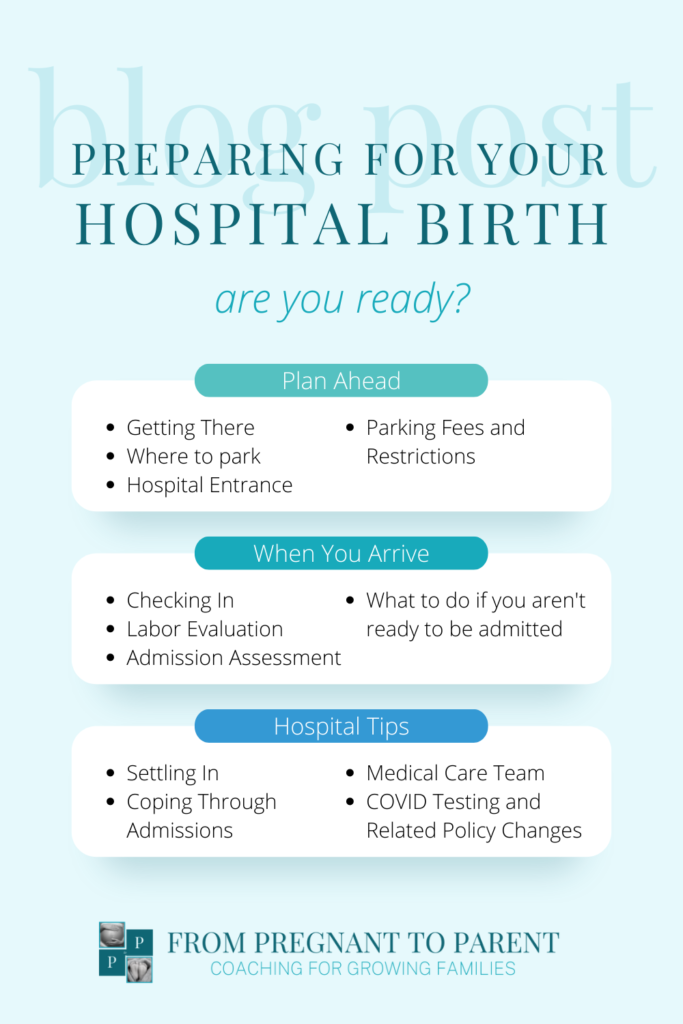
Preparing for Your Hospital Birth
You’ve probably thought about when and how you will go into labor. But have you thought about what comes next? If you’re planning on a hospital birth, it’s helpful to prepare for the drive and intake process so you can minimize logistical distractions and stay focused on your labor. Here’s a rundown of what to expect to help you prepare:
Planning Ahead for Your Hospital Birth
Well before your labor begins, make sure you know where to go when it’s time:
- How You’ll Get There: Make sure you have a plan for how you’ll get to the hospital and who will help you get there. Who will drive you? Would you rather have someone drop you off? Do you need a “Plan B” for certain times when your birth partner may not be immediately available to drive you (e.g., during work hours or planned travel)? What if you go into labor early? Having a backup plan can help eliminate extra stress in the event of the unexpected.
- Hospital Entrance: Make sure you know what entrance to use and if there’s a different “after-hours” entrance. Many hospitals have a main entrance for use during the day and an emergency entrance to use during the night.
- Where to Park: Do you know where to park your car when you arrive? See if there is a short-term parking area by the entrance where you can park when you first arrive. This will save you from having to navigate a long walk across a large parking lot while coping with contractions.
- Parking Fees: Avoid surprise parking fees or unexpected tickets by researching parking information well before you arrive. If you’re taking a hospital tour, that’s a great time to ask about any parking limits or restrictions, fees, and validation options. Not taking a hospital tour? Check the hospital’s website or call the main hospital line.
When You First Arrive
Checking In
When you first get to the hospital, leave your bags in the car and head towards check-in with the bare essentials. If you’re having a hard time walking during contractions, don’t be afraid to stop and cope however you need to. You can also have your partner get a wheelchair for you as soon as you arrive and skip the walk if that feels more comfortable.
Depending on your hospital and the time of day, you may have to check in at a security desk before you are directed to Labor & Delivery (aka L&D).
Once you get to the L&D registration desk, an admitting nurse will check you in, confirm your identity, help you fill out any necessary paperwork, and give you your hospital ID bracelet. Many hospitals allow you to pre-register online to help expedite this process so you aren’t trying to fill out paperwork while coping with labor.
Labor Evaluation
In some instances, such as a scheduled c-section, patients are directly admitted to the hospital. However, most birthing parents can expect to have a labor evaluation done before they’re admitted to Labor & Delivery.
At many hospitals, a nurse, OB, or midwife will do this preliminary assessment in a nearby triage exam room. They will check your and your baby’s vitals, check your baby’s position in relation to your pelvis, ask about your contraction pattern and any additional symptoms you’re experiencing, and monitor your labor.
To avoid an increased risk of infection, cervical checks are often avoided unless there’s a clear medical need. If your bag of waters is still intact, your provider will likely want to check for cervical readiness (effacement, softness, position, and dilation) to help determine if you’re ready to be admitted. Keep in mind, you have the right to refuse (or request) cervical checks during pregnancy and labor if that’s your preference.
If you suspect your bag of waters has broken, there is an increased risk of infection. A sterilized speculum is used to obtain an amniotic fluid sample for confirmation, but your provider will likely skip the cervical check.
Your provider will then weigh how you’re progressing with how far you live from the hospital and how well you’re coping to decide if you’re ready to be admitted.
If You’re Not Admitted
If your care team decides you’re not ready to be admitted, you’ll be instructed to come back when your labor has progressed further. Try not to be discouraged! It can be mentally beneficial to change the scenery during labor. A long labor can feel even longer when you’re stuck in the same room for hours (or days).
Leaving will also give you the freedom to cope with early labor in whatever way feels best to you. Choose someplace familiar where you feel safe and mentally relaxed. Your home, a local park, a nearby restaurant, the grocery store, or even Target might be that place for you.
The key to coping with early labor is to distract yourself! That’s often easier to do away from the hustle and bustle, beeping machines, and bright lights. So, eat a light meal, go for a walk, binge a favorite show, and try not to hyperfocus on your contractions!

Settling In For Your Hospital Birth
Once you’re admitted, a nurse will escort you from the triage exam room to your labor room. In many hospitals, you’ll labor and deliver your baby in the same room. At some hospitals, you’ll recover in this same room as well! This is a great time for your birth partner to get the rest of your personal belongings from the car.
Your nurse will then do a more extensive admission exam to assess how your labor is progressing and how your baby is coping. During this exam, you can expect to be hooked up for about 20-30 minutes of continuous fetal monitoring. Your nurse will also ask more detailed questions about your medical history, collect blood and urine samples, offer you a hospital gown, and orient you to your room.
You likely won’t need an IV when you are first admitted, but your nurse will likely offer you a heparin lock. Your nurse will place an IV catheter near your wrist, add a drop of heparin to prevent blood clotting, and “lock” the catheter instead of hooking it p to an IV machine. This allows your care team to act quickly with IV medication or fluids in the event of an emergency, so you aren’t unnecessarily tethered to an IV pole.
Your Medical Care Team
After you’re admitted, a primary nurse will be assigned as your main point of contact for the duration of their shift (typically 8 – 12 hours). Depending on the size of your hospital and how busy the unit is, your nurse will likely need to assist with other patients during their shift, so you can expect them to be in and out of your labor room, especially while you are in the early and active phases of your labor.
You and your birth partner will have lots of time alone during your labor, which is one of the reasons why hiring a doula and having a pre-planned coping strategy can be so beneficial. Don’t be afraid to press that call button to ask your nurse for additional support and coping suggestions when you need them.
Your OB or midwife may pop in for brief visits before your baby is born, or you may not see them until just before your baby is born. This is especially true if your delivery is low-risk and remains free of complications. Throughout your labor, your primary nurse will be giving them updates on your progress, asking questions, and/or raising any concerns.
On rare occasions, the assigned primary nurse just isn’t a good fit. In those instances, it’s important to know that you have the option to request a different primary nurse. Just ask to speak to the charge nurse or a patient advocate and let them know what’s going on.
COVID Testing and Related Policies
We have seen policies change rapidly over the last couple of years. At many hospitals, there are visitor restrictions, testing and masking requirements, and/or impacts on pain relief options. During one of your final prenatal appointments, check in with your OB about this. Ask about any COVID related policies and if there have been any recent changes to your hospital’s policies.
Coping Through Admission
Have you heard a story about someone going to the hospital absolutely certain they’re in active labor only to have contractions slow down or stop? It’s a fairly common story! The reason for this is often adrenaline.
There are many hormones involved in the labor process, but a few, in particular, are important to understand. Oxytocin (the love hormone) tells your uterus to contract. Beta-endorphins provide natural pain relief. Melatonin (the sleep hormone) supports and potentially enhances oxytocin. And adrenaline (the “fight or flight” hormone) counteracts oxytocin.
You may feel a variety of emotions during the drive to the hospital. For example, fear, excitement, anticipation, stress, anxiety, happiness, or relief are all common. Some of those feelings are more helpful than others. Try to shift your focus away from any adrenaline-producing thoughts or feelings as much as you can. Instead, replace those thoughts with positive affirmations. Calming your mind and body (even just a little bit) will help to promote oxytocin release.
In the car, get as comfortable as you safely can. Then, focus on coping with the labor you’re experiencing rather than worrying about what’s ahead. Focus on your breath. Listen to feel-good music. Seek loving touches from your birth partner. And, keep the lights dim–even as you’re packing the car and driving to the hospital.
You can prepare for this moment by practicing your coping techniques anytime you’re riding in the car during pregnancy. By practicing in the car, you’ll help to create some familiarity in your body and build muscle memory so the techniques come a bit easier when you need them.
Settling Into Labor
As your labor progresses and contractions build, you’ll find that you need more and more of your focus for coping. During the check-in process (and beyond), your birth partner can help you stay focused by answering questions on your behalf. Set them up for success by telling them about key components of your medical history before you go into labor.
Remember, motion is the lotion of labor. Throughout your hospital birth, don’t feel like you have to just lay in bed. Move your body as much as you can in ways that feel good to you. Ask for a birth ball if you want one. Labor in your own clothes if you don’t want to wear a hospital gown. Try getting the shower or birth tub if you have one available to you. If you have access to the hallways and other parts of the hospital, go for a walk. Or, just pace, sway, dance, and move about your room.
Every step of the way, try to stay in the moment. There’s no way of knowing exactly how your labor will unfold. So, cope with the labor your are experiencing right now, not the labor you anticipate is coming. Share your feelings with your partner. Ask for help when you need it. Listen to your body. Trust your instincts. You are prepared for this moment!
Still have questions?
Do you still have questions about how to prepare for birth, develop your own coping strategy, or decide on your birth preferences? Our team of caring, professional coaches is here to help! Supporting growing families through the transition into parenthood is our passion. Click here to set up a coaching call and learn more.
- About the Author
- Latest Posts

Richelle’s passion is supporting growing families through the unpredictable and transformative journey of pregnancy and the first years of parenthood. In 2019, she set out with a vision to create a modern-day parenting village: From Pregnant to Parent. In addition to being our founder, she is a certified doula, childbirth and lactation educator, sleep coach, and RETAIN parental leave coach. When she isn’t working, she enjoys spending time with her husband and two kiddos around their home in Marin County (San Francisco Bay Area).
Sources
https://health.clevelandclinic.org/prenatal-appointment-schedule/
- About the Author
- Latest Posts

Richelle’s passion is supporting growing families through the unpredictable and transformative journey of pregnancy and the first years of parenthood. In 2019, she set out with a vision to create a modern-day parenting village: From Pregnant to Parent. In addition to being our founder, she is a certified doula, childbirth and lactation educator, sleep coach, and RETAIN parental leave coach. When she isn’t working, she enjoys spending time with her husband and two kiddos around their home in Marin County (San Francisco Bay Area).
November 27, 2022
Richelle Clayton
A Note About Links: Our blog is reader supported. When you buy a product through the links on our site, we may earn a small affiliate commission. We promise, we only recommend products we genuinely like. Purchasing through our links doesn't effect the price you pay, but it does help to support our small business.
Leave a Reply Cancel reply
FTC Affiliate Disclosure: When you purchase through the links on our site, we may earn an affiliate commission at no extra cost to you. By doing so, you don't pay a higher price, but you do help to support our small business. If we ever promote something that was gifted to us, we'll be sure to say so. Regardless of whether or not we are earning a commission, we promise, we will only ever recommend products we genuinely like and use (or would use) ourselves.
Follow Me
On Instagram
Tips | Updates | Behind the Scenes
CLick Here
RESOURCES
RESOURCES
CONTACT
CONTACT
FOR PARENTS
FOR PARENTS
FOR PREGNANCY
FOR PREGNANCY
GET TO KNOW ME
HOME